Submitted by achenault on Wed, 01/14/2015 – 1:50pm
As we move through the current Open Enrollment period, many Ohioans are seeking out assistance to help them understand the enrollment process and get covered. In the first month of the current open enrollment period, 89,000 Ohioans signed up for coverage through the Marketplace.
UHCAN Ohio Certified Application Counselors (CACs), who are located in churches and community-based organizations across the state, are seeing another aspect of Open Enrollment as well. In addition to new enrollees, our CAC sites are also seeing an increase in the numbers of people with existing coverage who are now coming back with questions on re-enrollment and how to use their coverage. Marsha Riley, one of our Columbus-based CACs, states that about 40-50% of those she sees are people she helped last year.
“This is very encouraging, because it shows that our system of using trusted messengers located at community based sites to provide enrollment assistance and follow-up is working,” says Nita Carter, UHCAN Ohio’s Director of outreach and enrollment.
The goal of our project that builds enrollment assistance capacity in African American and other underserved communities is to make sure that people not only get covered but use their coverage to get connected to needed care. “Having people with questions about how to use their insurance is exciting. That means they are not just placing that card on a shelf someplace. They are really using it,” says Carter.
With funding from the Robert Wood Johnson Foundation, UHCAN Ohio has partnered with churches and community based organizations as well as Enroll America to open 22 sites in Cleveland, Columbus and Cincinnati. These sites will remain open after the enrollment period ends to provide follow-up, assist with Medicaid enrollments, answer questions, and help people understand how to use their coverage and get the right care at the right time and place.
For more information on the sites, go to enrollmenthelp.
Submitted by achenault on Fri, 02/13/2015 – 3:59pm
 Ohio Department of Medicaid (ODM) has taken action to terminate thousands of Medicaid recipients who have not responded to recent requests for information. Here’s what people need to know:
Ohio Department of Medicaid (ODM) has taken action to terminate thousands of Medicaid recipients who have not responded to recent requests for information. Here’s what people need to know:
ODM is required to verify continued eligibility for most people on Medicaid every 12 months. This process is called “Medicaid Redetermination,” “Recertification,” or “Renewal”. Each month starting in January, ODM is sending enrollees a 14-page packet to complete. Many people did not receive their packets due to incorrect addresses.
Recipients who receive a packet can renew their benefits by supplying the required information in one of the following ways:
What to Do if You Receive a Letter Terminating Your Benefits
If the renewal information is not received on time, Medicaid recipients will receive a letter terminating (ending) their benefits. People who get a termination letter have 90 days to appeal the decision. If the hearing officer decides in your favor, your Medicaid will be reinstated and it will be retroactive – your medical bills for those 90 days will be covered.
If you appeal within the first 15 days, you get to keep your Medicaid while waiting for the appeal. You will probably get your Medicaid back faster if you appeal within the 90 days rather than re-apply.
If you miss the 90-day deadline, you can re-apply for Medicaid.
People who need help renewing their eligibility or getting their benefits back should contact their local legal aid office or a Certified Application Counselor or Navigator who provides enrollment assistance. To find your local legal aid office, go to http://bit.ly/1A0pT4y or call 1-866-529-6446,
Here are the five items you can use to talk with Medicaid customers:
1. If the customer states they received a re-determination/recertification packet, they need to complete it to the best of their abilities, then mail the packet to the address on the top of the front page of the letter. There is no envelope so they need to mail the packet in their own envelope and the amount of postage required is about 70 cents to be on the safe side.
2. If the customer no longer has the packet or is unable to fill it out or mail it, they will have to walk into a county Job and Family Service office or call the county office and renew at the JFS office.
3. If the customer has received a termination notice they have 90 days from the date of termination to recertify. During this period the customer’s Medicaid will not be active so they need to recertify and the Medicaid will be retroactive up to 90 days.
4. It is not necessarily in the best interest of the customer to reapply as a new applicant unless the 90 days from the date of determination is over. This may slow down their Medicaid more.
5. In many instances this should be treated in the same way as previous Medicaid recertification in terms of documents and household information.
Submitted by achenault on Tue, 08/25/2015 – 10:08am
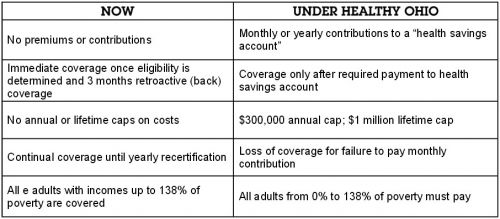
In the new Ohio 2-year budget, the Ohio legislature proposes to create a new health care program for most people on Medicaid. It is called “Healthy Ohio,” but names can be deceiving. If approved, Healthy Ohio will restrict access to health care for many thousands of low income adults.
The good news is that the federal government must give Ohio permission to make such radical changes in Medicaid, and public input matters.
Under the proposal, all non-disabled adults over age 18 with incomes up to 138% of the poverty level will be required to enroll in “Healthy Ohio” if they are on Medicaid.
How Healthy Ohio would change health care:
|
NOW |
UNDER HEALTHY OHIO |
|
No premiums or contributions |
Monthly or yearly contributions to a “health savings account” |
|
Immediate coverage once eligibility is determined and 3 months retroactive (back) coverage |
Coverage only after required payment to health savings account |
|
No annual or lifetime caps on costs |
$300,000 annual cap; $1 million lifetime cap |
|
Continual coverage until yearly recertification |
Loss of coverage for failure to pay monthly contribution |
|
All adults with incomes up to 138% of poverty are covered |
All adults from 0% to 138% of poverty must pay |
What’s Wrong with “Healthy Ohio?”
Healthy Ohio will lead to poorer health for Ohioans on Medicaid. So many people will lose coverage that the state will estimate the cost of the program based on the assumption that many Ohioans will lose their Medicaid. That’s because studies show that requiring even small contributions prevent low income people from accessing health care. Many people will lose coverage and seek care – often in emergency departments – only when they are sicker and more expensive to treat.
Healthy Ohio is complicated:
Healthy Ohio is a Big Waste of Taxpayer Money. Setting up and operating the debit card and point system will cost millions of dollars that could be spent more wisely.
What’s Next? The Ohio Department of Medicaid is responsible for applying to the federal government – Centers for Medicaid and Medicare Services – for permission to change the way Ohio operates Medicaid now.
Two Important Opportunities to Weigh In On Proposed Changes to Ohio Medicaid: People concerned about changes to Ohio’s Medicaid program have two chances to express their concerns and ask regulators to reject Ohio’s request.
Bottom line: Ohio’s current expanded Medicaid program is working well. It has made health care a reality for hundreds of thousands of low income Ohioans. Ohio Medicaid helps Ohioans get and keep employment, stabilizes their families, and helps them stay healthy. Making it harder for Medicaid enrollees to get the health care they need will take us in the wrong direction.
If you want to have an information session on “Healthy Ohio,” contact Kelsey Raines at UHCAN Ohio.
Submitted by achenault on Wed, 11/18/2015 – 3:34pm
Many supporters of Ohio’s Medicaid expansion are confident that the Obama administration’s Center for Medicaid and Medicare Services (CMS) will reject Ohio’s application to implement “Healthy Ohio” for most Ohio adults on Medicaid. (For more on “Healthy Ohio,” click here.)
After all, unlike most other states requesting waivers, Ohio has been implementing the Medicaid expansion since January 2014 and it’s been an overwhelming success, with over 600,000 now receiving regular health care. And the Kasich administration tried to steer legislators away from putting such a complex proposal in statute, wishing instead to have flexibility to negotiate something less onerous than “Healthy Ohio.”
However, recent decisions from CMS granting Medicaid waivers with major beneficiary restrictions should give pause to supporters of Ohio’s Medicaid expansion who believe that Ohio’s application will be dead on arrival. On November 2, CMS approved Montana’s Medicaid waiver, which expands Medicaid eligibility but requires recipients to pay premiums amounting to two percent of their income. Worse, these premiums are applicable to people with incomes at or above 50% of the federal poverty level (that’s $5885 a year for one person). Individuals between 100-138% FPL could lose coverage if they are more than 90 days late on premiums and they would be locked out for one quarter if they fail to pay back owed premiums. These and other provisions will cause people to lose their coverage and not return until they get sick. Cost sharing will keep people from seeking needed preventative care in a timely basis.
The approval by CMS of a waiver very similar to Ohio’s is a warning to opponents of Healthy Ohio that we can’t be too confident that CMS will reject “Healthy Ohio” application – at least not without hearing from a wide range of stakeholders why this waiver is not in Ohio’s best interests. However, there is a key difference between the situations in Ohio and Montana: Ohio has already successfully expanded Medicaid, whereas the approval of Montana’s waiver will put expanded Medicaid into effect on January 1, 2016. Since Ohio’s expansion of Medicaid does not rely on the waiver’s approval, advocates can argue that Ohio already has a working system in place and does not need the additional changes in the waiver.
On the other hand, Arizona has requested a waiver with provisions similar to those found in other states – premiums for people with low incomes, cost sharing, and provisions requiring enrollees to take certain actions to demonstrate “personal responsibility.” Like Ohio, Arizona already implemented the Medicaid expansion and politicians are seeking to impose more “personal responsibility” – that is, hurdles – in the paths of low-income people on Medicaid. Public comments on the Arizona waiver are due on December 6. UHCAN Ohio will be submitting comments; others are encouraged to do so as well.
In Ohio, the administration plans to submit its application by spring of 2016. Before filing with CMS, they are required to seek public comments. Then, after submitting the application, CMS opens up a public comment period. Supporters of Medicaid expansion across the spectrum – providers, consumers, and other stakeholders – need to be ready to join UHCAN Ohio in sending a strong message to CMS that Healthy Ohio is bad for Ohioans.
On the Brighter Side…
In this blog, Community Catalyst offers evidence that “reason is slowly gaining ground over ideology in the debate over Medicaid expansions.”
Submitted by achenault on Tue, 12/15/2015 – 3:34pm
With Ohio’s proposed Healthy Ohio waiver threatening the future effectiveness of expanded Medicaid, Ohio advocates are keeping a close watch on the outcome of Medicaid waivers in other states. UHCAN Ohio joined a coalition of Ohio advocacy organizations to submit comments to Centers for Medicare & Medicaid Services (CMS) on Arizona’s proposed waiver, which would have similar effects to Healthy Ohio.
Arizona is the first state to request a waiver after already implementing expanded Medicaid. In both Ohio and Arizona, expanded Medicaid has successfully decreased the uninsured rate and made it possible for thousands of low-income adults to get health coverage. 630,000 Ohioans have obtained coverage due to expanded eligibility since January 2014, allowing them to obtain regular care.
Like Ohio, Arizona’s proposed waiver features premiums for all adults on Medicaid, regardless of income, potential loss of coverage for missed payments, complicated “health savings accounts,” and benefit limits. These requirements create barriers that will keep people from enrolling or cause people to lose coverage and will increase the cost of administering the program.
If Arizona’s waiver is approved by CMS, it will set a precedent that will make it more likely that Ohio’s waiver will also be approved. These waivers, if approved, will cause many low income people in Ohio and Arizona to lose health coverage. That’s why Ohio advocacy organizations are calling on CMS to reject Arizona’s proposed waiver.
In the letter, the advocates state that “The Affordable Care Act is one of the most significant legislative and policy initiatives of our lifetimes. It promises all Americans access to health care. We should protect that promise and not allow it to be eroded into a shadow of itself. For all of these reasons, we request that [the Department of Health and Human Services] reject the Arizona application as submitted.”
Click here to read the full letter, and click here to read additional comments on Arizona’s waiver by Families USA.
Submitted by achenault on Tue, 01/12/2016 – 3:25pm
Since Ohio expanded Medicaid eligibility, over 647,000 Ohioans have gained health coverage. Now the State would like to make changes to the Medicaid program which could affect over 2 million adults and children currently enrolled in Medicaid. The Ohio Department of Medicaid (ODM) is preparing to submit a waiver to the Centers for Medicare and Medicaid Services (CMS) seeking approval for several changes to Ohio’s Medicaid program. Here are the changes the “Healthy Ohio” waiver would make:
These changes will create huge barriers for people trying to maintain health coverage and obtain timely, needed health services. All of the research says that these measures will cause people to drop from the rolls of Medicaid, undoing the successes of Ohio’s Medicaid expansion.
The good news is Ohioans and organizations that serve Ohioans who would be negatively impacted by these changes have two opportunities to weigh in before CMS decides to approve or deny the waiver.
Now is the time get informed about what the waiver is, how it will affect you and/or your constituents, and develop a plan for you to participate in the public comment periods.
Click here for resources to learn more about the waiver, including a new introduction letter you can send to your network.
Click here to join our Healthy Ohio Action team to get the latest updates on the waiver and learn more about how you can get involved.