Submitted by achenault on Tue, 04/07/2015 – 5:27pm
People on Medicaid need to keep a watchful eye out for an eligibility re-determination notice coming from the County Department of Job and Family Services (ODJFS). Consumers missing the notice risk having their benefits terminated! (a lawsuit challenging the redetermination process is now pending – see other article).
The annual redetermination process has resumed in January 2015, after being halted for the entire year of 2014 to allow for the Medicaid expansion and other changes to be implemented. The delayed 2014 notices and annual notices for January through April 2015 have now been sent out to Medicaid recipients, which includes MyCare Ohio (dually eligible) enrollees as well as all others on Medicaid for more than one year. The Ohio Consumer Voice for Integrated Care (OCVIC) has heard from enrollees wanting to understand the significance of this document. All Medicaid enrollees receiving Food Assistance, cash, medical, or any other benefit must go through this eligibility redetermination. It is very important to follow the instructions provided, or seek assistance. If you do not, your benefits may stop. Please take the necessary steps to avoid any service disruptions in food or medical assistance.
Need help with your Medicaid renewal?
Submitted by achenault on Tue, 04/07/2015 – 5:21pm
UHCAN Ohio has been building outreach and enrollment capacity in communities of color by working with churches and community organizations to strengthen their ability to navigate the uninsured from their congregations and communities to coverage. We would like to highlight two of these programs: Horn of Africa Voluntary Youth Committee (HAVOYOCO), in Columbus, and University Settlement, Cleveland. HAVOYOCO primarily serves Africans, including the Somali population. University Settlement serves primarily African Americans and, through its partners, also serves Hispanic populations.
With funding from UHCAN Ohio’s Robert Wood Johnson Foundation Consumer Voices for Coverage grant, these two programs operated multiple enrollment sites and were able to hire and provide stipends to Certified Application Counselors (CACs) from their communities to provide outreach, enrollment, and post-enrollment activities for the communities they serve. The stipends allowed the programs to recruit people who had a passion for working in their own community. “We tried to do this work last year with volunteers. We had some volunteers, but did not have the quality of people who provided regular hours we could count on. We had much more success using stipends. Our CACs’ enrollment hours were more consistent, they conducted regular outreach and enrollment, and they came up with innovative places to conduct outreach and enrollment,” said Belinda Harris, CTSOC Lead Parent Advocate at University Settlement.
HAVOYOCO operated two community sites and funded two African enrollment assistors. University Settlement operated four community sites and funded three African American assistors. During the months of November through January, HAVOYOCO and University Settlement CACs provided face-to-face enrollment assistance to over 300 persons, many of whom spoke English as a second language, and conducted outreach to more than 500. More important than the numbers is the fact that there are now five trained CACs who are providing continuing enrollment assistance, following up with those they assist to make sure they got the coverage they need and understand how to use it, and who are prepared to steer people from their communities to coverage during the current special enrollment period and the next open enrollment period.
If you or someone you know needs coverage, contact us at 614 456-0060 ext. 233 or click here.
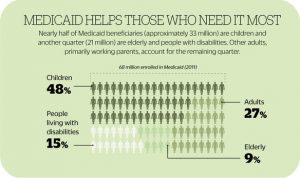
 This morning, UHCAN Ohio joined with Enroll America, the Ohio Hospital Association, and the Ohio Association of Community Health Centers on a press conference call celebrating the 50th anniversary of Medicaid becoming law and discussing the progress made through Ohio’s expanded Medicaid program.
This morning, UHCAN Ohio joined with Enroll America, the Ohio Hospital Association, and the Ohio Association of Community Health Centers on a press conference call celebrating the 50th anniversary of Medicaid becoming law and discussing the progress made through Ohio’s expanded Medicaid program.
Earlier this week, we shared the importance of Medicaid to the health of Ohioans. The Ohio Medicaid Program is one of the great success stories in health care, providing nearly 3 million Ohioans the health care they need in a timely, efficient, and effective manner. Medicaid covers low-income parents, veterans, people struggling with mental illness and addiction, and others who need health care but can’t afford it. The expansion of Medicaid in Ohio has allowed low-income adults to access needed medical care, including preventative care to keep small issues from turning into serious, expensive illnesses.
The Affordable Care Act offers states the opportunity to expand Medicaid to include more low-income individuals and families who would previously not have been eligible. UHCAN Ohio embraced the opportunity to expand Medicaid to all low income adults, and the broadest coalition of stakeholders ever seen in Ohio came together to support the Governor in enacting the expansion of Medicaid. Ohio’s expansion of Medicaid allows adults between the ages of 19 and 64 with incomes below 138% of the Federal Poverty Level to receive Medicaid benefits. Since the Medicaid expansion went into effect in January 2014, 596,000 new Ohioans enrolled in Medicaid, contributing to a total 2.9 million current Medicaid enrollees in Ohio. Click here for more information on how Medicaid is working in Ohio.
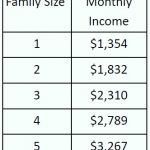
 People can apply for Medicaid at any time – there is no open enrollment period for Medicaid. Ohioans can go to benefits.ohio.gov to check their eligibility or apply. Free in-person application assistance is also available: visit connector.getcoveredamerica.org or call 1-800-648-1176 to find help near you. See the table for Medicaid income limits by household size.
People can apply for Medicaid at any time – there is no open enrollment period for Medicaid. Ohioans can go to benefits.ohio.gov to check their eligibility or apply. Free in-person application assistance is also available: visit connector.getcoveredamerica.org or call 1-800-648-1176 to find help near you. See the table for Medicaid income limits by household size.
UHCAN Ohio is proud to advocate for the Medicaid program, including its expansion that has allowed low-income Ohioans to get the care they need when they need it to be healthy and productive. We’re happy to join our partners in celebrating the 50th anniversary of this effective, cost-efficient program that improves the health and well-being of Ohioans.
The Affordable Care Act offers states the opportunity to expand Medicaid to include more low-income individuals and families who would previously not have been eligible. UHCAN Ohio embraced the opportunity to expand Medicaid to all low income adults, and the broadest coalition of stakeholders ever seen in Ohio came together to support the Governor in enacting the expansion of Medicaid. Ohio’s expansion of Medicaid allows adults between the ages of 19 and 64 with incomes below 138% of the Federal Poverty Level to receive Medicaid benefits. Since the Medicaid expansion went into effect in January 2014, 596,000 new Ohioans enrolled in Medicaid, contributing to a total 2.9 million current Medicaid enrollees in Ohio. Click here for more information on how Medicaid is working in Ohio.
People can apply for Medicaid at any time – there is no open enrollment period for Medicaid. Ohioans can go to benefits.ohio.gov to check their eligibility or apply. Free in-person application assistance is also available: visit connector.getcoveredamerica.org or call 1-800-648-1176 to find help near you. See the table for Medicaid income limits by household size.
 UHCAN Ohio is proud to advocate for the Medicaid program, including its expansion that has allowed low-income Ohioans to get the care they need when they need it to be healthy and productive. We’re happy to join our partners in celebrating the 50th anniversary of this effective, cost-efficient program that improves the health and well-being of Ohioans.
UHCAN Ohio is proud to advocate for the Medicaid program, including its expansion that has allowed low-income Ohioans to get the care they need when they need it to be healthy and productive. We’re happy to join our partners in celebrating the 50th anniversary of this effective, cost-efficient program that improves the health and well-being of Ohioans.
Submitted by clevine on Tue, 11/26/2013 – 3:40pm
By: Cathy Levine, Executive Director, UHCAN Ohio
Great news! As of January 1, 2014, more immigrants living in Ohio who are here with legal documentation will be eligible for Medicaid just like citizen residents. Note: this does not change the ineligibility of persons without legal documents for Medicaid except for emergency Medicaid
Ohio has been one of the most restrictive states, denying Medicaid to legal residents who would otherwise be eligible for Medicaid – low income families, pregnant women, people with disabilities and seniors, simply because they are not citizens. Federal law bars legal non-citizen residents for five years, but most states treat them like citizens after the five years. But not Ohio. The situation has put enormous stresses on families, and economic burdens on those health providers who treat people regardless of ability to pay, including hospitals and community health centers. Thus, this change is great news.
This change also applies to individuals who came to the U.S. as refugees or asylees and have used up their 7 years of Medicaid eligibility but have not yet become citizens.
In addition, pregnant women and children permanent residents are eligible without the five year waiting period as soon as they become permanent residents.
The applicable rule is Ohio Administrative Code 5101:1-37-58.3 Medicaid: Non-Citizens.
Congratulations to Columbus Legal Aid attorney (and UHCAN Ohio board member) Kate McGarvey and others for bringing the lawsuit which helped to bring about this change, as well as other health advocates who have pushed to eliminate this discriminatory barrier to Medicaid.
Submitted by kgmeiner on Tue, 02/04/2014 – 2:56pm
By: Kathleen Gmeiner, Project Director, OCHC
Three Republican Senators – Orrin Hatch, Tom Coburn and Richard Burr – introduced on January 27, 2014 the Republican replacement plan to go with their party’s call to “repeal and replace Obamacare.” It’s called the “Patient Choice, Affordability, Responsibility, and Empowerment Act (CARE Act).” It would be a very poor replacement for the ACA. It makes health care affordable for far fewer people and at the expense of comprehensive benefits and covering those excluded from the market by pre-existing conditions. Here is what it does:
People would have protection from insurance company discrimination based on pre-existing conditions ONLY IF they were continuously insured. Otherwise their option would be state high risk pools that the law would aid. [Note: State-run high risk pools have never been effective in covering the millions with pre-existing conditions].
Young adults could still remain on their parents’ insurance policies.
Prohibition on lifetime limits in what an insurance company will pay out remains.
People who fail to choose a health plan would be passively enrolled in a plan at the subsidy to which they are entitled; they could drop it.
It would encourage malpractice reform.
It would give states Medicaid dollars based on the number of people enrolled in Medicaid, not based on what the state spent on Medicaid. The ACA provision that subsidizes states at 100% and then down to 90% would be gone. Persons eligible for Medicaid could take Medicaid or buy private insurance instead with a subsidy.
It would keep the changes to Medicare in the ACA.
It would prevent insurance companies from canceling insurance policies except for fraud or misrepresentation.
What’s missing from the Republican plan?
The mandated set of benefits (The ACA requires policies to have ten essential health benefits)
The prohibition against gender discrimination
Protection for pre-Medicare age older adults –Under the ACA, a 60-year-old cannot be charged more than 3 times what a 20–year-old is charged. Under the Republican plan, the older person could be charged 5 times as much. And, states could even opt out and charge greater than five to one.
Tax subsidies are cut off at 300% of the federal poverty level, not 400% as under the ACA
Financing – the insurance, hospital and medical device provider taxes that support the ACA are gone; the replacement is a reduction on what employers who provide insurance can deduct from their taxes.
The Center for Health and Economy, a newly-created think tank by former Congressional Budget Office and Republican Douglas Holtz-Eakin, issued a fiscal analysis of the plan January 30th. Of note, the Center says that “there will be a significant increase in individual market participation, but that is “expected to be offset by large reductions in the Medicaid population.” (emphasis added)
And that’s the rub. While the plan would provide subsidies, it would greatly reduce Medicaid. And it leaves all of the people with pre-existing conditions who are unable to maintain continuous coverage at the mercy of state high risk pools, which have a terrible track record for helping large numbers of those with pre-existing conditions. Those who could maintain coverage would likely do so with higher deductible plans that would not be required to provide mental health and substance use disorder services, maternity coverage, women’s health benefits and the preventive services – all now firmly established in the ACA.
Let’s take a look at the subsidy in the ACA and the CARE Act by looking at a hypothetical.
Tricia is 26-year-old single adult living in Franklin County with annual income of $22,000, or 191% of the federal poverty level. Under the newly proposed “CARE” Act she would get a subsidy of $1,560 for a year. Applied to the lowest cost silver plan in the current Ohio Marketplace, she would pay $125 per month under CARE, while under the ACA she is paying $105. But, under the ACA she can receive, without co-pay or deductible, an annual well woman visit and a routine Pap test. Under the ACA, if she gets pregnant she’s covered. If she is diagnosed with a mental illness, she’s covered. Under Tricia’s silver plan she can see her doctor for a $10 co-pay. None of these benefits is guaranteed in the CARE plan. And without the ACA, she may be paying more for her insurance than a 26 year old male living in her same city.
There is one silver lining in the introduction of this new plan. It shows that Republicans recognize that they can’t keep calling for the ACA’s repeal without an alternative and that to have a chance at passing a “replacement” bill, they cannot totally roll back the ACA. But that is about the only positive that can be said about it.
Submitted by achenault on Wed, 01/14/2015 – 1:56pm
On January 5, 2015, new members of Ohio’s 129th General Assembly were sworn in with their first task on the horizon – the biennial budget. Capital Bureau Chief Mark Kovac provides a great top 10 list of Things to Know About the Start of Ohio’s New General Assembly. The list shares changes in leadership, new members of the General Assembly, and details about possible legislation and budget issues.
One of the big issues to watch is Ohio Medicaid. Starting on January 1, 2014, Medicaid became available to all Ohioans (except some immigrants) and whose income falls below 138% of the Federal Poverty Level (FPL). To date, over 450,000 Ohioans have enrolled in Medicaid coverage thanks to the expanded eligibility.
Gov. Kasich is expected to present his budget on February 2nd, keeping the current income eligibility requirements for Ohio Medicaid intact. Then the next steps are:
Confused yet? You’re in luck!
If you’d like to learn more about Ohio’s budget process, the issues being considered, and how you can make a difference, join One Ohio Now’s webinar on Tuesday, January 27th from 12-12:45pm. Click here for more information and to register.
What’s this Mean for Advocates and Consumers?
We’ve seen the Medicaid Expansion in action for a year, and it has improved the lives and health of many Ohioans. We’ve got to start laying the groundwork now to preempt any attacks on it this budget season. Telling the stories of those who benefited from expanded Medicaid coverage is going to be key.
What Can You Do?
Have you or someone you know benefited from expanded Medicaid coverage? Or are you a trusted community leader? Right now our goal is to get as many Letters to the Editor as possible published across Ohio, specifically outside of the 3 C’s. We can help you write and submit your Letter to the Editor. Click here to view 3 sample templates. Click here to find the contact information for your local paper. Need more help? Email Alyssa at achenault@uhcanohio.org for more information or help writing/sending your letter.