
Submitted by achenault on Tue, 01/12/2016 – 3:25pm
Since Ohio expanded Medicaid eligibility, over 647,000 Ohioans have gained health coverage. Now the State would like to make changes to the Medicaid program which could affect over 2 million adults and children currently enrolled in Medicaid. The Ohio Department of Medicaid (ODM) is preparing to submit a waiver to the Centers for Medicare and Medicaid Services (CMS) seeking approval for several changes to Ohio’s Medicaid program. Here are the changes the “Healthy Ohio” waiver would make:
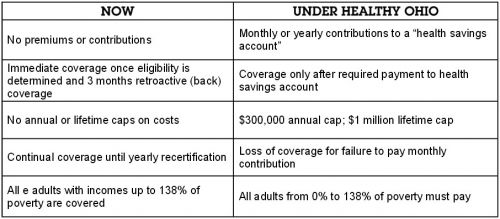
These changes will create huge barriers for people trying to maintain health coverage and obtain timely, needed health services. All of the research says that these measures will cause people to drop from the rolls of Medicaid, undoing the successes of Ohio’s Medicaid expansion.
The good news is Ohioans and organizations that serve Ohioans who would be negatively impacted by these changes have two opportunities to weigh in before CMS decides to approve or deny the waiver.
Now is the time get informed about what the waiver is, how it will affect you and/or your constituents, and develop a plan for you to participate in the public comment periods.
Click here for resources to learn more about the waiver, including a new introduction letter you can send to your network.
Click here to join our Healthy Ohio Action team to get the latest updates on the waiver and learn more about how you can get involved.
Submitted by achenault on Tue, 01/12/2016 – 3:29pm
A little role reversal, please.
Imagine for a moment, in the relationship between you and your dentist, that you are the dentist. Imagine as a small business owner (your dentist), you hear this:
These findings are exactly what legislators in Minnesota heard from the Minnesota Department of Health and the state’s Dental Board after an evaluation of dental therapists operating there as members of the dentist-led team.
Now imagine that as you are considering these findings, you also hear that:
Wouldn’t you think: “It is time to give me and other Ohio dentists the choice to be able to provide more quality, affordable, accessible dental care to Ohioans that need it!” We at Dental Access Now!, including several dentists from across the state, think so. Sign up for our Day at the Statehouse on February 24th to tell your legislator why dentists should have a choice to hire a dental therapist to improve dental access in Ohio.
Submitted by achenault on Tue, 01/26/2016 – 2:24pm
 Consumer input CAN change our health care system for the better. In a recent blog, we shared how our survey of MyCare Ohio enrollees’ experiences informed decisions to improve care coordination and the availability of all services, supplies, and equipment. We’ve continued to use the survey findings to advocate for changes to make health care work better for all MyCare Ohio enrollees, and we’re happy to share another success!
Consumer input CAN change our health care system for the better. In a recent blog, we shared how our survey of MyCare Ohio enrollees’ experiences informed decisions to improve care coordination and the availability of all services, supplies, and equipment. We’ve continued to use the survey findings to advocate for changes to make health care work better for all MyCare Ohio enrollees, and we’re happy to share another success!
Ohio Consumer Voice for Integrated Care (OCVIC) is UHCAN Ohio’s statewide coalition that is working to improve the care of older adults and people with disabilities enrolled in MyCare Ohio by bringing the voice of consumers to the Ohio Department of Medicaid (ODM) and Managed Care Organizations (MCOs). Our efforts influenced the Ohio Department of Medicaid to create a new measurement that guides the Managed Care Organizations to reduce the time it takes to approve a request or process an appeal for Durable Medical Equipment (DME). Our survey identified this as a problem for many enrollees, showing that:
80% of respondents reported that they require the use of DME, yet 73% stated they did not receive a needed upgrade or replacement in a timely manner.
This change means enrollees will get their needed equipment faster or their appeal processed faster.
Thanks to the all the people who distributed the survey and the over 3,000 enrollees who shared their concerns and experiences. Together we can get Ohioans the care they need to lead healthier lives through an organized consumer voice. To join the coalition or learn more about what OCVIC is doing, contact John Arnold.
Submitted by achenault on Tue, 02/02/2016 – 5:31pm
As we move toward UHCAN Ohio’s Day at the Statehouse, when we will to ask our legislature to allow Dental Therapists to practice in Ohio to address the lack of access to dental care, it is important to provide answers to the most pressing questions often raised about the dental therapist.
When the issue of adding new health professionals (e.g. nurse practitioners, physician assistants) to the physician-led team surfaced, Ohio providers at first vigorously fought the new professionals, eventually acquiesced, and then over time recognized that nurse practitioners and physician assistants were essential to the provider team. During the debates, the issues of education and supervision were raised about these new providers. When it comes to dental therapists in Ohio, organized dentistry is still in the fighting stage, but we know it’s only a matter of time before dental therapists are as celebrated as nurse practitioners and physician assistants.
The adequate training and education of Ohio’s future dental therapist students was addressed recently when the Commission on Dental Accreditation (CODA) agreed to implement education standards, which were approved last February. This landmark CODA decision followed by several years the development of a curriculum for dental therapists commissioned by the American Association of Public Health Dentists and completed by a group of the country’s most esteemed dental educators.
Regarding the concern about supervision, which typically stems from our proposal to allow the dental therapist to operate under general (remote) supervision or not under direct supervision of the dentist, the following restrictions should be considered:
In all cases, the supervising dentist will choose:
We trust that Ohio’s licensed dentists have been adequately vetted, well-educated, and properly licensed and are capable of making the kinds of hiring and supervisory decisions which will best meet the needs of their patients.
While these questions require evidence-based answers, there is little question about the lack of access to routine dental care for many Ohioans. There are 84 areas all across Ohio that are already identified by the Ohio Department of Health as Dental Health Professional Shortage Areas. These HPSAs include most Appalachian counties, parts of rural northwestern Ohio, much of southwest Ohio, and parts of every major metropolitan community in the state. By definition, these are areas where there just aren’t enough dentists to meet the community’s needs. Dental therapists will make it easier for children and families in underserved communities to get high-quality, affordable dental care where they live.
Submitted by clevine on Thu, 07/28/2011 – 1:58pm
Have you ever had the same medical test repeated twice or more because your different doctors didn’t share the test results? Have you left a doctor’s office confused about what was said or what you were supposed to do? Did you ever feel like you didn’t have all the information you needed to make a decision about surgery or other treatment? Join the club.
Older Adults and Others with Multiple Chronic Conditions Get Uneven Care That Costs Too Much
The problems described above are particularly frequent for older adults and other people with chronic health conditions. In fact, fragmented, uncoordinated care and poor communications among doctors and between doctors and patients contributes to our nation’s high health care costs and uneven outcomes.
Likewise, many emergency department visits and hospitalizations for people with chronic illnesses could be avoided if the patient had better coordination and communication – what is often called, “Patient-centered care.” The Campaign for Better Care has developed “Eight Keys to Better Care,” to state clearly what older adults want from their care.
Patient-Centered Care is the Solution – But Will the Patient be At the Center?
Providers and payers are struggling to develop new models of care that do a more effective job at keeping people with chronic health conditions healthy and out of the hospital. Doing so will improve patient and population health, as well as dramatically lowering health care costs. But can providers and payers (insurers and employers) design more patient-centered care without input from patients?
If you’ve ever heard a doctor complain about patients who don’t follow their instructions or don’t show up for appointments, you’ll know that doctors don’t always know what it’s like to be at the other end of the stethoscope – or what’s getting in the way of patient “compliance.” We need to make sure that older adults and family caregivers, as well as patient advocates, have real input into the design of “patient-centered” primary care models.
New Models of Care Are Being Created Across Ohio – Will Patients and Families Have a Voice?
Efforts to develop patient-centered primary care for patients with chronic conditions are going on in Cincinnati (Aligning Forces for Quality, a project of the Cincinnati Health Improvement Collaborative of Greater Cincinnati), Cleveland (Better Health Greater Cleveland) and Columbus (Access HealthColumbus Primary Care Collaborative), as well as in Ohio’s Medicaid program (the Health Homes Initiative). At the same time, hospitals across the state are engaged in patient safety initiatives, spurred by the HHS “Partnership for Patients.”
The Ohio Campaign for Better Care wants all of these patient-centered primary care and patient safety initiatives to have a strong, effective voice of patients and family caregivers involved in designing and giving input into the model. We’re calling for Patient/Family Advisory Councils (or “PFACs”).
Sign Up to Join the Ohio Campaign for Better Care and get involved with bringing PFACs to Ohio!.
Submitted by clevine on Sun, 08/14/2011 – 2:45pm
“If you don’t understand how to achieve lower costs, listen to the stories of patients – poor care coordination, ineffective care,” said Dr. Donald Berwick, at a Campaign for Better Care event on Wednesday, August 10, in Cincinnati.
Dr. Berwick, administrator for CMMS (Centers for Medicare and Medicaid Services), addressing a roundtable of 100 providers and advocates in Cincinnati, said that quality improvement is the route to lower costs. The event was organized by the Campaign for Better Care, which is working to ensure that health care reform improves care for older adults with chronic conditions. UHCAN Ohio is the lead organization for Ohio Campaign for Better Care. Go to our website for more information.
Dr. Berwick stated: the alternative to quality improvement – cutting care for people on Medicare and Medicaid – will lead us in the wrong direction. He also opposes turning Medicare into a voucher program. Instead, he is promoting better care coordination, especially for the 77% of Medicare patients with chronic health conditions. Those with multiple chronic conditions tend to be the heaviest users of health care, with the worst outcomes, and highest costs. If we can improve care for them, we can achieve real savings.
Dr. Berwick’s associate, Dr. Paul McGann, explained HHS’ Partnership for Patients, a new campaign involving federal and state governments, hospitals, physicians, health plans, and consumers to improve patient safety. We waste billions of dollars each year on preventable hospitalizations and re-hospitalizations for preventable conditions. The goals of P4P are to reducing hospital readmissions by 20 percent and hospital-acquired conditions by 40 percent by 2013.
The Cincinnati patient safety event will available, by videocast, on the UHCAN Ohio website soon.